You might remember that are my yearly appointment in 2022, my team told me that I had to—definitely—start an exercise program.
Up until that point, I’d never really had one. I’d done some things sporadically, I’d done a 5K the year after my transplant, and I’d gone to barre, ballet, and yoga classes on and off. But I’d never really had a set program that I did consistently.
Now it was time to get one.
Today I’m going to walk you through my program, do some before and afters, and talk about general fitness-y things.
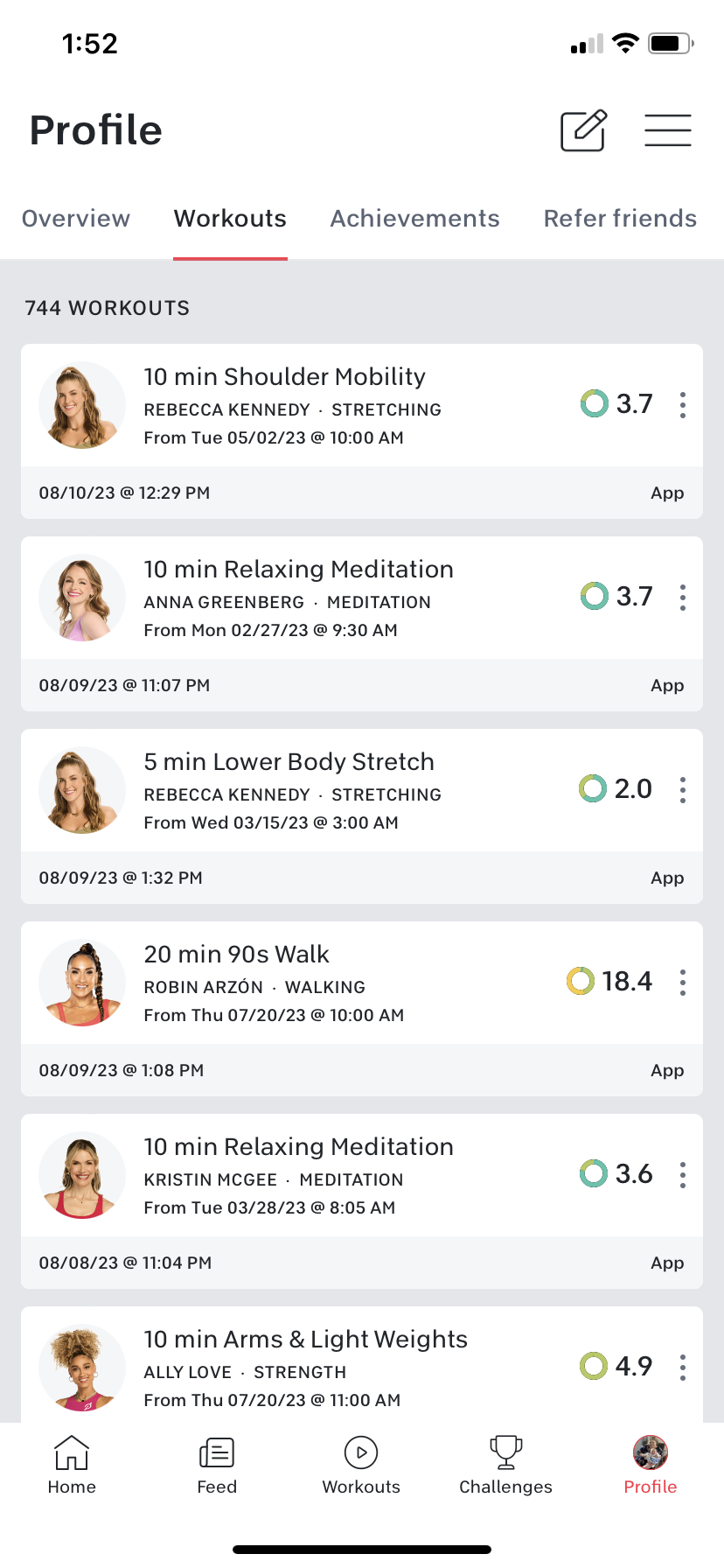
The first thing I did was sign up for the Peloton app. Two things, right off the bat:
This post is in no way sponsored by Peloton. It’s what works for me so I’m talking about it, but I don’t get paid to say any of this.
I do not have any of the Peloton equipment (the bike, the tread, the row). I use the app exclusively, and use the treadmill in my complex gym for my walks.
The “super goal” as it’s called in the goal setting world, is to be working out every day for 30 minutes, with one rest day (Sunday) per week.
I was starting at zero, so this goal is still in progress. I am working out almost every day, but not for 30 minutes, generally.
As I’ve talked about before, my body is weird. I have about 54% lung function, which is good for me, but it’s half of a normal person’s. I have a wonky right knee and right Achilles’ tendon, as well as tight hamstrings. I say this to lay out what I am dealing with and how my routine has helped me here.
So, all that aside, here’s how it goes:
I break my workouts down into several areas: cardio (swimming, yoga, walks), strength, stretching and mobility, and I use the peloton meditation classes. (I don’t meditate, per se. I use these to help with stress and relaxation before bed, because keeping stress low/manageable is a big part of keeping blood glucose levels in check.)
For cardio: I do the treadmill walks on the app—usually 20 minutes, but sometimes 15 if my day is packed and I need to get a workout in. I have done one 30 minute session so far.
When I first started—being totally honest here—I could barely hit 1.0 on the treadmill. Now I’m at 2. (On my treadmill. The app says I’m going about 2.5 on my speed, but speed varies on treadmills).
When I first started, I couldn’t follow any instructor cues (to go faster or to increase incline). Now, I do follow them (within reason—I’m not ready for 6 or 8% incline—yet), and I like them. The app also offers hikes, which I’m going to try for the first time this week! The highest incline I’ve hit so far is 4%.
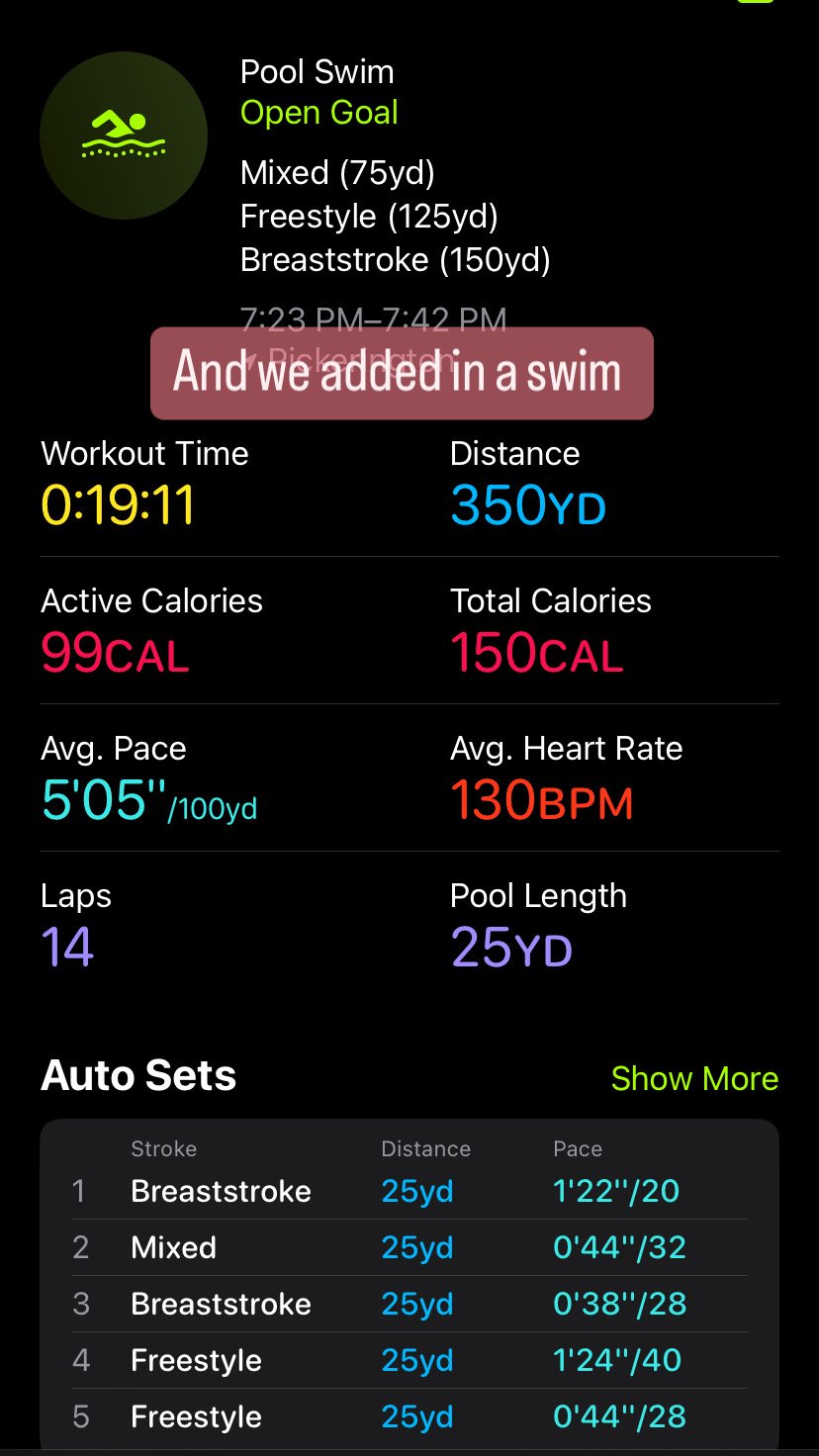
I also swim in the complex pool, which is a little harder to do regularly, because I have to have room to swim, and in a shared pool, that can be hard to do. I don’t swim fast enough to feel comfortable at a Y or JCC pool doing laps. As you can see above I’ve started tracking my swims with my Apple Watch. I’m hoping the pool will be open for a few more weeks so I can get in more sessions, because swimming really is my favorite cardio. (It’s generally open May-September.)
I count yoga as cardio; I know some people don’t, but when you have the lung function I have, even slow flow classes count for getting the heart rate up. I’m trying to be more consistent here after doing a week long yoga program on the app earlier this summer. There are a wide variety of classes. I almost always do a restorative yoga class once a week because these are great for opening up my chest (very important in the pulmonary world), releasing tight areas, and also reducing stress. (There is actual science that backs up how yoga can help lots of health conditions, CF being one of them; check out the book Yoga as Medicine* for more on this.) Obviously restorative yoga is not cardio, but my body really likes it.
A look at the yoga classes I’ve taken.
For strength, I do the 10 minute arms and light weights on the app. For these you use 1-3 pound weights, with the objective being lower weights but higher reps. I’m currently using the 2 pound weights and I might be ready for the threes, so that’s a huge improvement from the no weights I used when I first started. I love these classes. I’ve dropped a shirt size since I’ve started doing these.
For leg and core exercises (which are also works in all the other things I do) I do things like wall sits, plies, pelvic tilts, etc.
Stretching and mobility is also really important to me. I always do a lower body stretch after a treadmill session and I stretch out my arms after weights. Sometimes I do a really focused 10 or 20 minute stretch like you see above with the “hip mobility”. My legs get very cranky if they do not get stretched out regularly.
Here’s what this looks like in a normal week:
Monday: Restorative Yoga
Tuesday: 10 minute arms and light weights
Wednesday: Treadmill session with stretch after
Thursday: 10 minute arms and light weights
Friday: Treadmill session, restorative yoga.
Saturday: 10 minute arms and light weights.
Stretching and swims are added in as possible.
I want to add in more dedicated yoga classes, possibly on T or Th, and I also want to experiment with some other strength classes on the app.
I am much stronger and fitter than I was a year ago, an I can’t wait to see what gains I can accomplish in the next year!